Background
Minimal residual disease (MRD) is currently considered as one of the most powerful predictors in patients with Philadelphia chromosome-negative acute lymphoblastic leukemia (Ph - ALL).The time points and thresholds for MRD monitoring in pediatric Ph - ALL have been well established. However, surveillance strategy in adult ALL has not yet been standardized. In this study, we explored the prognostic value of MRD levels and monitoring time points by flow cytometry (FCM) in adolescent and adult patients with Ph - ALL treated with pediatric-inspired regimen.
Methods
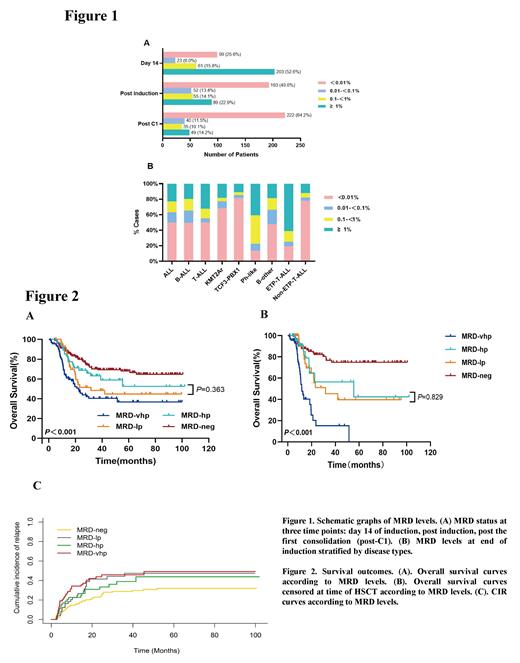
This analysis includes adolescent and adult patients who were treated according to a pediatric-inspired regimen revised based on Children's Oncology Group protocol (CCG-1961). This prospective study was registered at Chinese Clinical Trial Registry Website with the registration number of ChiCTR-OOC-15006328. MRD was measured using bone marrow aspirates with eight-color multiparametric FCM on day 14 of induction, at end of induction (EOI, days 29-42) , post the first consolidation (post-C1), and throughout the treatment period. MRD was defined as the percentage of lymphoblasts present in the total nucleated cells counted. MRD levels of < 0.01% and ≥ 0.01% was considered as negative and positive, respectively.Patients who were MRD-positive were further stratified into three groups according to MRD level: MRD low positive (MRD-lp), ≥ 0.01% to < 0.1%; MRD high positive (MRD-hp), ≥ 0.1% to < 1%; and MRD very high positive (MRD-vhp), ≥ 1%.
Results
From 2014 to 2021, a total of 415 patients with a median age of 27 (range: 14-69) years were treated. Three hundred and twelve patients presented with B-precursor ALL and 103 with T-cell ALL. With a median follow-up time of 40.8 months, the median overall survival (OS) of the cohort has not yet been reached. There were 386, 389, and 346 BM samples available for MRD evaluation on day 14 of induction, at EOI, and post-C1, respectively. Figure 1A presents the distribution of MRD status over time. Figure 1B depicts the compositions of MRD levels at EOI stratified according to disease types. Notably, Ph-like ALL and early T-cell precursor (ETP) ALL were associated with extremely lower achievements of MRD negativity at EOI compared with other types. The 5-year OS rates of patients with MRD negativity, MRD-lp, MRD-hp, and MRD-vhp at EOI were 68.0% (95% CI: 60.2%-75.8%), 44.8% (95% CI: 28.9%-60.7%), 52.4% (95% CI: 34.2%-70.6%), and 36.7% (95% CI: 24.2%-49.2%), respectively ( P < 0.001) (Figure 2A). If patients were censored at the time of hematopoietic stem cell transplantation, the 5-year OS rates of these patients were 74.9% (95% CI: 65.1%-84.7%), 39.7% (95% CI: 18.7%-60.7%), 42.3% (95% CI: 11.7%-72.9%) and 0%, respectively ( P < 0.001) (Figure 2B). Patients with a negative MRD at EOI had a more favorable OS than those with a positive MRD at EOI. There was no statistically significant difference in terms of survival time between patients with MRD-lp and MRD-hp. Further, patients with MRD-vhp had the worst survival. The relapse probabilities had a similar pattern. Patients with MRD negativity at EOI had a lower 5-year CIR than those with MRD positivity at any levels. Compared to MRD-lp and MRD-hp patients, patients with MRD-vhp experienced a significantly higher rate of early relapse. However, with a longer follow-up, the 5-year cumulative incidence of relapse (CIR) did not differ significantly among patients with a positive MRD in any of the three groups, with a rate of 47.4%, 43.8%, and 49.1% in patients with MRD-lp, MRD-hp, and MRD-vhp, respectively (Figure 2C). Multivariate analysis showed that positive post-induction MRD was one of independent predictors of both OS and Disease-free survival.
Conclusion
Our study confirmed that MRD negativity at EOI is an independent prognostic factor of OS in adolescent and adult patients with Ph - ALL treated with pediatric-inspired regimen. Patients with MRD-lp and MRD-hp at EOI had a lower OS and a higher relapse incidence than those with MRD negativity. Therefore, an early and deep MRD clearance is important, and even extremely low MRD levels can predict poor prognosis.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal